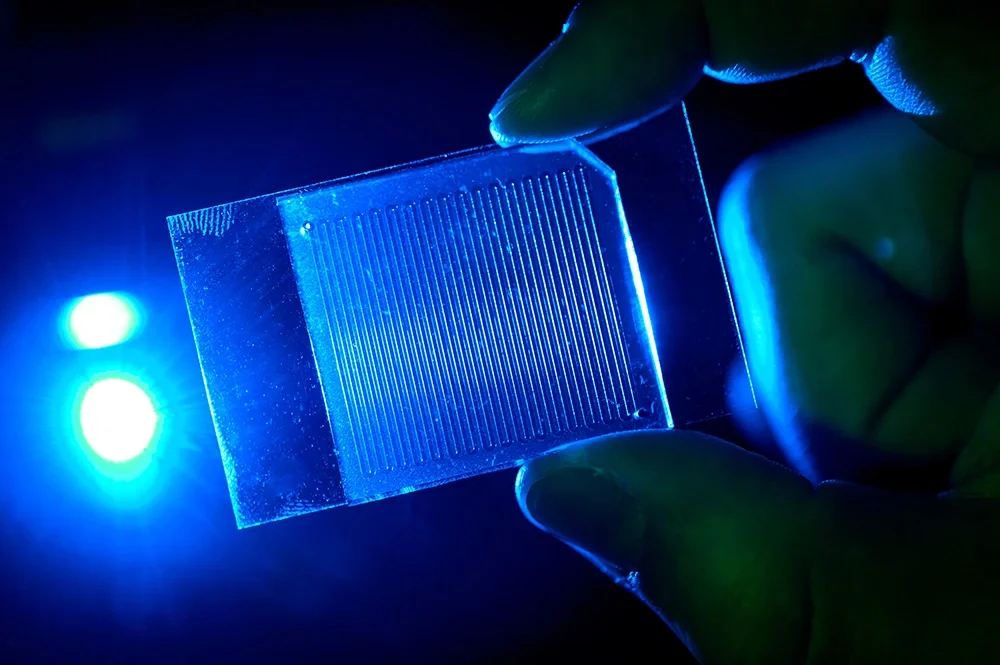
Some notoriously difficult to treat infections may not be as resistant to antibiotics as has been thought, according to new research using a microfluidic device that more closely duplicates the fluid flow found in the body than standard cultures.
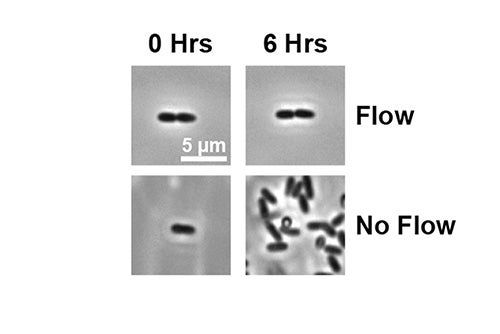
The University of Illinois Urbana-Champaign research team, led by biochemistry professor Joe Sanfilippo, tested antibiotic agents against Pseudomonas aeruginosa, considered one of the most highly resistant pathogens. They introduced the drugs at varying rates of fluid flow and found that, while the bacteria thrived at no or low fluid flow, the antibiotics killed the bacteria at higher flow rates.
“Anytime you take an antibiotic orally or by IV, it’s not immediately in the place it is supposed to be. It will get there by flowing in the bloodstream. Other fluids move throughout the body as well: in the lungs, the urinary tract, the digestive tract. Yet biologists don’t really study the impact of fluid flow when they study pathogens,” Sanfilippo said. ”By using this microfluidic technology, often used in engineering, in a biology setting, we found that fluid flow is very important for antibiotic activity. We have an opportunity to make our drug screening and testing better by considering the effects of fluid flow.”
(Images by Alexander Shuppara.)
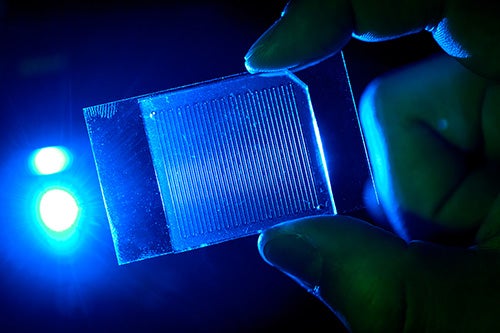
Whether in a biology lab or a clinical lab, the standard way to study pathogenic bacteria is in plates, tubes or wells — settings not representative of the dynamics found in the body. The microfluidic devices the Illinois group used allow for precise control of the rate of fluid flowing.
“It’s a simple idea. Biologists just haven’t done it because it’s hard to achieve with what they usually have in their labs. The engineering is pretty simple, in terms of microfluidic design. We just had to put the technology and biology sides together,” Sanfilippo said.
The researchers tested three different antibiotic agents against which the Pseudomonas was supposedly resistant. They saw a gradient of antibiotic activity that was dependent on the flow rate. At no to low flow, the antibiotics affected only the bacteria at the very start of the fluid track. As the flow rate increased, so did the reach of the antibiotic activity, until the entire culture sample was wiped out at the highest tested flow rates.
The team published its results in the journal Science Advances.
“Our findings highlight how we could do a better job of characterizing antibiotic resistance. If you get an infection, a clinician might take a sample and test it to see which drugs will work against it. But they’re testing it without flow. So they may not give you a drug that actually could be effective because their tests don’t show how effective the drugs are in flow conditions like in the body,” Sanfilippo said. “When researchers try to develop a new drug, it’s the same thing; they might be wrong in interpreting whether the drug is working or not, because the testing conditions aren’t like the body.”
Next, the research team plans to test other antibiotic-resistant pathogens and other antibiotic drugs in their microfluidic devices. They also hope to more deeply study the mechanisms behind why the antibiotics were more effective in flowing fluid.
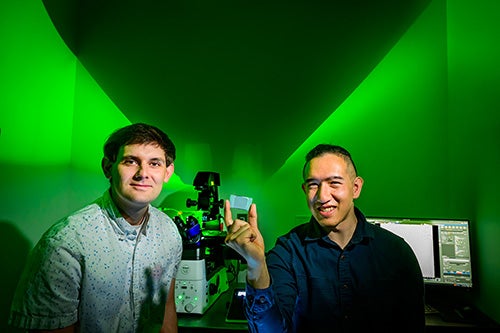
The University of Illinois and the National Institutes of Health supported this work. Graduate student Alexander Shuppara was the first author of the paper.