It was the early 1980s. At the time, glioblastoma patients survived on average for only 10-11 months. Four decades later, the life expectancy has only marginally improved by a few months.
For one team of scientists, these aren’t just statistics but family history. Though their grandfather died in the early 1980s, the shared childhood memory of his battle with glioblastoma (GBM) motivates the work of two cancer researchers—scientists whose mothers are twin sisters. It is this personal history and clinical urgency that brought chemical and biomolecular engineering professor Brendan Harley, Cancer Center at Illinois (CCIL) program leader, and Rebecca Riggins, associate professor of oncology and associate director of education and training at Georgetown Lombardi’s Comprehensive Cancer Center, together to tackle one of cancer’s most deadly manifestations.
While Harley and Riggins are first cousins, this close familial bond and shared genetic composition didn’t guarantee a future of synergistic scientific pursuits. It was only recently, in 2020, that Brendan and Rebecca’s scientific paths serendipitously crossed.
Harley’s journey into cancer research began with bioengineering—a healthcare-focused vocation he chose because of his childhood leukemia diagnosis. He began developing tissue engineering models to regenerate implantable tissues for the body, but in the early 2000s there was no vision of using such models to study cancer.
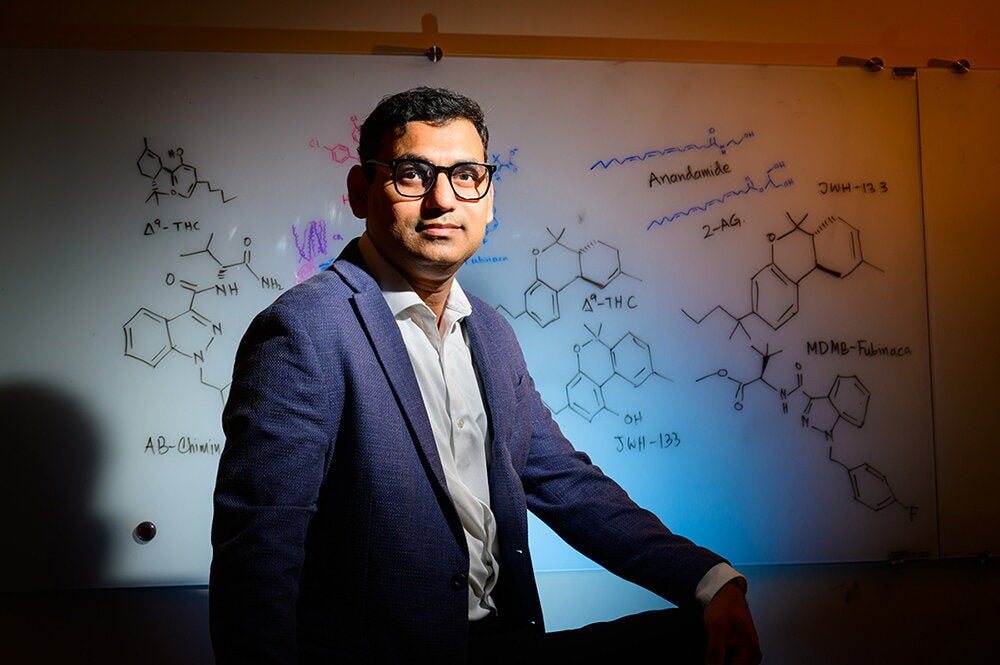
“I was fortunate to come to Illinois to start a lab focused on regenerative medicine. I began working on growing stem cells and tissue models. Then, about fifteen years ago, I presented a seminar at a National Institutes of Health (NIH) workshop on the potential efficacy of tissue engineering models for the study of cancer progression. By happenstance, there was someone at Illinois studying GBM at that time who wanted to grow GBM cells outside the body,” said Harley. Since then, Harley’s lab has continued building its GBM research focus and has earned a series of NIH grants to investigate the GBM matrix environment.
Riggins established herself in the cancer research space earlier than Harley. While Harley’s strengths lie in bioengineering and tissue modeling, Riggins’ expertise is in molecular biology and breast cancer genomics. These differing scientific roles are what made Harley and Riggins excellent teammates for their current investigation of GBM.
“My lab studies proteins called nuclear receptors and their communication with genes, particularly in the context of breast cancer. We’re focused on what is happening inside the cells, asking questions like: What are the molecules, proteins, and communication signals that make cancer cells aggressive? Can we turn these off? Are there drugs we can apply or other strategies to reduce the aggression? We’ve been doing this for over a decade, focused on breast cancer. But one of my graduate students had a desire to study this protein activity in GBM, also due to family history. So, we began to explore what we are seeing in breast cancer that we also observe in GBM?” shared Riggins.
With their trains unexpectedly running in parallel, the two cousins realized it made sense to link up. So, they applied for an NIH R01 grant to study GBM and received their first award in 2020, in the heat of the pandemic. “I remember getting that call while sitting in my car. It was a tremendous boost, because it was such a difficult time during the pandemic—as a human and scientist. And now, four years later, here we are with our second NIH grant to keep moving our GBM research forward,” remarked Riggins.
The research duo’s first NIH grant supported their development of brain tumor microenvironment hydrogel models to study brain vasculature and patterns of cancer invasion and response to the frontline GBM drug, temozolomide (TMZ). The team relies on cell lines developed in Riggin’s lab and patient-derived tissue samples from Mayo Clinic. To date, the two labs have developed a validated vascular model and are studying drug response in vivo.
With that foundation, the Harley and Riggins team recently applied for and received a second NIH R01 grant. This time, the team has an even more robust goal in mind: to investigate potential new targets and compounds to treat GBM.
“The current GBM survival rates are just not acceptable with TMZ,” said Harley pointedly.
But that honest assessment alone isn’t enough to warrant a second NIH grant. “What provoked this additional GBM research project was that Becca had a surprise in her lab,” said Harley. “While looking at an estrogen receptor beta molecule in her breast cancer research, she found high amounts of a variant of that receptor expressed in high amounts in long-term GBM survivors. Not only is this isoform expressed in survivors, but she also saw that GBM cells showed a degree of growth arrest where this molecule was present. The cancer cells weren’t proliferating as fast. So, with her study of this receptor using a zebrafish model (a translucent fish), we are using our lab’s hydrogel models to study invasion, proliferation, and gene expression. We’re testing this intriguing receptor, hoping to identify some underlying molecular mechanisms.”
The team doesn’t have a drug target yet but believes they may discover how this noteworthy receptor is a central regulator of GBM proliferation and invasion. This study will help the team explore the mechanisms by which a subset of GBM patients produces this receptor in high quantities and ideally identify a new target and potential new compound.
Because cancer operates like an ecosystem of different kinds of cells with different communication pathways, the challenges within the brain environment for GBM patients are particularly pernicious.
“GBM kills you because we don’t yet understand how it spreads, and we can’t target the cells that spread beyond surgical margins. Many cancers are lethal when they metastasize—spreading to alternate sites. You combat that with better imaging, diagnostic, and surgical tools. GBM doesn’t really metastasize, but the problem with surgical procedures is that you are cutting into the brain. You obviously can’t remove all the brain, so those remaining cancer cells at the surgical margin are pernicious; they come back to haunt you,” commented Harley. “With this newest grant, our two labs will develop tools to study the processes involved in the cancer cell invasion and proliferation, hopefully identifying better target and a better anti-cancer compound that will open the door to longer survival times for patients suffering from GBM,” said Harley.
“We want to better understand the cancer ecosystem, including other cell types, blood vessels, the immune system, and more. Our goal is to build a multi-cellular model of GBM to understand its behavior and how the drug affects that larger ecosystem. It’s a more expansive project that could push our understanding of GBM forward and lead to more effective treatments,” added Riggins. “I never imagined that I would get to collaborate scientifically with family. There was never a grand scheme to arrive at this stage, but I feel very privileged to do this work—scientifically and personally meaningful work. This project highlights how essential collaboration is in cancer research. The CCIL brings expertise in bioengineering, model systems, and computing; we bring our strengths in molecular biology and cancer host interactions. We’re better together, and I look forward to working with the CCIL more in the future,” concluded Riggins.